Modification of proximal row carpectomy (PRC) technique for adaptive wrist collapse
Translation of publications into other languages is carried out technically
Original article https://doi.org/10.18019/1028-4427-2024-30-4-502-510
CLINICAL EXAMPLE
Modification of proximal row carpectomy (PRC) technique for adaptive wrist collapse
Sh.K. Kuttygul, D.E. Tyagunov, N.A. Shchudlo
Ilizarov National Medical Research Centre for Traumatology and Orthopedics, Kurgan, Russian Federation
Corresponding author: Shyngys K. Kuttygul, artana.kaz@gmail.com
Abstract
Introduction Proximal carpal row resection has been used for many decades as a “salvage procedure” for progressive wrist collapse. Improving the technique of its implementation, as well as introducing various modifications of the technique into practice are an important area for achieving better results of surgical treatment.
INTRODUCTION
A pain-free and stable wrist joint is essential for full hand function. In clinical practice, patients frequently refer with pain at the wrist level, the causes of which are conventionally divided into mechanical, neurological and systemic. The most common cause of chronic pain is osteoarthritis of the wrist, which is classified into inflammatory, degenerative, infectious and hemorrhagic. Primary idiopathic osteoarthritis of the wrist (osteoarthritis) is a rare condition, while secondary osteoarthritis occurs after simple trauma, instability, dislocations, or inflammatory arthritis resulting from cerebral palsy, penetrating gunshot wounds, and infections.
Secondary degenerative arthritis of the wrist frequently results from injuries to the scapholunate ligament or fractures of the scaphoid followed by nonunion or malunion. Subsequently, adaptive collapse of the wrist may develop, a pathological condition consisting of a progressive disruption of the anatomically correct relative position of the bones and their fragments or rows of bones of the wrist, leading to a decrease in height, changes in biomechanics and a high rate of degenerative process. Wrist collapse should be considered as a unique outcome of instability, which has a long-standing nature that will aggravate the course of post-traumatic osteoarthritis.
One of the main tasks of a hand surgeon is to restore the anatomical and functional integrity of the damaged segment and relieve pain, and the surgeon has various types of surgical interventions for this purpose. The choice of treatment method depends on the cause and nature of the consequences of the causing pathology and the needs of the patient. Available procedures can be grouped into two main treatment options, namely partial or complete wrist arthrodesis and wrist arthroplasty, as well as palliative and salvage treatments.
To relieve chronic carpal pain syndrome, decompression of the bone marrow cavity of the distal end of the radius is used, aimed at improving its blood supply, as well as partial or complete denervation of the wrist, which can be independent operations or complement others.
A common surgical technique for various degenerative conditions is resection of the proximal row of carpal bones. It refers to operations that preserve the range of motion (as opposed to total arthrodesis, when movement in the joint is sacrificed). Resection of the proximal row of carpal bones has several advantages: relative ease of execution, shorter duration of postoperative immobilization, and no risk of bone nonunion, unlike arthrodesis. It can be used in patients who do not require greater handgrip strength. The consequence of the technique may be the process of osteoarthritis in the formed radiocapitate joint, which develops over time in most patients and is associated with heavy physical labor. It may subsequently require additional surgical interventions. Despite that resection of the proximal row of carpal bones is time-tested, the problem of improving the technique of its implementation remains relevant. It determined the purpose of our study.
Surgical technique
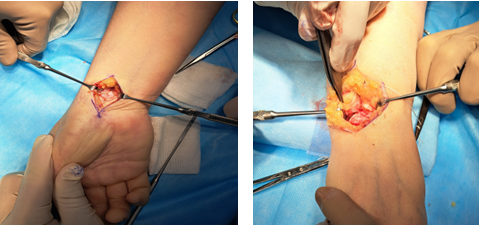
During the operation, conduction anesthesia was used. The patient’s position was supine with the arm on the bedside counter. After preparing the surgical field, a hemostatic pneumatic tourniquet was applied at the level of the middle third of the humerus. Surgical approach to the scaphoid bone was carried out from a 4–5 cm long incision along the anterior surface of the forearm, using the flexor carpi radialis (FCR) as an external landmark. After making the incision, the tendon was moved to the side for exposure of the capsule of the wrist joint and for examination of the articular surfaces of the distal radius and scaphoid bones (Fig. 1). Next, resection of the scaphoid bone was performed. To prevent impingement syndrome, resection of the styloid process of the radius was performed. Then, through an additional dorsal approach 4–5 cm long, the retinaculum extensorum was exposed and the 5th canal of extensors was opened. The extensor tendons of the fifth finger were moved to the side, the wrist capsule was incised along the dorsal radiocarpal ligament (DRC) (Fig. 2), and the distal radius and midcarpal joint were examined to ensure the integrity of the lunate fossa of the radius and capitate bones.
If they are damaged, an alternative to surgery must be considered. If there is any question regarding the correct identification of the carpal bones, fluoroscopy with a metal wire marker is an option. Removal of the triquetral and lunate bones is performed similarly to the removal of the scaphoid using surgical techniques.
 |
 |
| Fig. 1 Palmar approach | Fig. 2 Dorsal approach to the wrist |
Then X-ray control was carried out. The joint capsule was sutured with non-absorbable suture material in accordance with literature recommendations. After removing the tourniquet, thorough hemostasis was carried out and the wound was closed in layers with an interrupted or intradermal suture. In the case of perilunar dislocation and damage to the ligamentous apparatus, the wrist was immobilized in a functionally advantageous position using the Ilizarov apparatus. To do this, two wires were inserted crosswise in the lower third of the forearm and two wires were inserted in the middle third. The wires in the forearm were secured and tensioned in rings. The rings were connected to each other by straight rods. Two wires were drilled through the bases of the II–V metacarpal bones. The wires were fixed in a half ring. The half-ring and rings were connected by rods through hinges, providing a functionally advantageous position of the hand in relation to the forearm.
In the postoperative period, painkillers, dressings, antibiotic prophylaxis were prescribed; from the third day after the operation, exercise therapy was initiated.
Case report
A 36-year old patient aged complained of pain at rest and during exercise, limited movement in the left hand. An. morbi: domestic injury on 23.10.2021, bruise from falling on the hand. Perilunar dislocation of the hand was diagnosed at his residence hospital. Under local anesthesia, the dislocation was reduced and the hand and wrist joint were immobilized with a plaster splint. The follow-up radiographs detected that the dislocation had not been eliminated. The patient fixed his hand with an orthosis for two months and underwent physiotherapy courses. Due to persisting complaints, he was hospitalized at the National Ilizarov Medical Research Center for Traumatology and Orthopaedics on 09.03.2022.
The examination revealed chronic transscaphoid perilunate dislocation of the left hand, arthrosis, synovitis of the left wrist joint, and a nonunion of a comminuted fracture of the styloid process of the left ulna (Fig. 3–4).
 |
 |
| Fig. 3 Radiographs at admission | |
 |
 |
| Fig. 4 Function before surgery | |
Soft tissue contracture prevented reduction of the dislocation. On March 18, 2022, resection of the proximal row of carpal bones was performed, as well as resection of a fragment of the styloid process of the left radius with fixation of the hand and forearm in the Ilizarov frame (Fig. 5).
In the postoperative period, the pain severity decreased compared to the preoperative period and, due to fixation with the Ilizarov apparatus, no repeated subluxations or dislocations were noted. On April 12, 2022 (27 days after the operation), the device was removed. Subsequently, fixation with an orthosis was indicated for one month.
1 year after the operation, the volume of flexion and extension was 95°, of which 65° extension and 30° flexion (Fig. 6, 7).
 |
| Fig. 5 AP and lateral radiographs taken on day 1 Fig. 6 Treatment result. AP and lateral radiographs post-surgery at 1-year follow-up |
 |
 |
| Fig. 7 Photos of patient’s hand function at 1-year follow-up | |
Pain score according to VAS at rest and under loading was zero. The QuickDASH score was 13 points.
Hand grip strength was 2 points relative to a healthy hand.
DISCUSSION
Progressive narrowing of the joint space and arthrosis of the radiocapitate joint inevitably occur after PRC due to replacement of the complex carpal joint with a hinge joint.
In patients under forty-five years of age with increased functional demands, a balanced approach is required when choosing PRC or quadrilateral arthrodesis, depending on which functional parameters (grip strength or range of motion) are more important to the patient.
Chim et Moran in a 2012-study analyzed long-term results of PRC in 147 patients and reported an average result of postoperative range of motion (flexion and extension: 73.5°), which does not contradict our average results of range of motion, flexion and extension (67. 5 ± 18.3)°.
A special feature of our PRC technique is the presence of two mini-approaches. Unlike the conventional dorsal approach through the III–IV tendon canals, the use of two mini-approaches makes it easier to restore the integrity of the tendon canals and provides a better cosmetic effect, including by maintaining incisions along the Langer tension lines, which correspond to the natural orientation of the collagen fibers of the dermis. Such incisions usually heal better and cause less scarring, which is a significant factor in the prevention of desmogenic contractures. The use of the Ilizarov apparatus for chronic perilunar dislocations is also a new aspect of PRC modification, which has proven to be the technique of choice, providing high-quality immobilization of the wrist and reduction of pain in the postoperative period.
CONCLUSION
The analysis of the short-term results of the modified PRC technique shows that it reduces the invasiveness of the operation, improves the esthetic result, provides relief of pain at rest, a satisfactory range of motion and grip strength. The data obtained from eight patients treated are preliminary; further studies of short-term and long-term results will justify the introduction of the modified PRC technique into clinical practice.
Information about the authors:
Shyngys K. Kuttygul — post-graduate student, artana.kaz@gmail.com;
Denis E. Tyagunov — orthopaedic surgeon, head of the department;
Natalya A. Shchudlo — Doctor of Medical Sciences, leading researcher, nshchudlo@mail.ru.




Hello, is it possible to fix the wrist joint not with the Ilizarov apparatus, but with other methods?
Good article